The first detected COVID-19 was in Wuhan, China, in December 2019. Infection with SARS-CoV-2, an enveloped single-strand RNA virus, causes it. There have been a growing number of cases of individuals experiencing short-term first episodes of psychosis other than delirium at the time of, or shortly after, a positive SARS-CoV-2 examination.
The correlation between COVID-19 diagnosis and hysteria may be spurious, but the details support a causal link in many cases. Various aetiological mechanisms may be at work, including psychosocial stressors associated with inflammation, precipitating insanity in vulnerable people. Anxiety over one's health, fear of death, and social alienation are all examples of stressors. Quarantine has been shown to have negative psychological consequences such as anxiety and frustration. An Italian paper identified three patients who experienced their first mental disorder while being quarantined for COVID-19. Brief depressive symptoms have also occurred in individuals who have experienced psychiatric trauma due to the pandemic but have not been contaminated with SARS-CoV-2. Suicidal behaviour has been observed in some forms of psychosis. The psychotic illness caused by COVID-19 is discussed in this article.
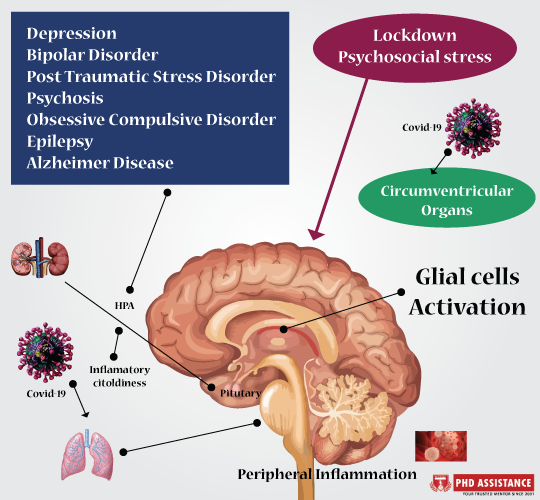
The accumulation of scientific
data has improved our understanding of the psychiatric characteristics of
cerebral illness through the years. In recent decades, research in viruses'
putative aetiologic presence has grown to include not only the organic
psychotic illnesses caused by acute viral encephalitis and sluggish viral
infections of the central nervous system (CNS) but also so-called functional,
psychological diseases such as insanity, depression, and bipolar disorder (BD).
It is now widely accepted that the combination of chronic infection, viral
neurotropism, and environmental trauma stimulates or even causes the emergence
of psychological pathologies, which intensify the trajectory of the pandemic
and pose a major therapeutic challenge. Viral infection of the brain may have various
physiological and psychological effects, leading to both the acute and
long-term effects of the disorder (Fig 1).
Figure 1. Illustration of virus causing a various effect to the brain
Psychosocial causes for psychiatric illnesses
- Furthermore, psychiatric illnesses that arise during the pandemic can be caused by psychosocial causes such as:
- The frequency and degree of exposure to people infected with the virus
- The fear of infecting family members
- Lack of access to COVID-19 testing and medical treatment.
- Physical segregation, home confinement, quarantining, and loneliness
- Inconsistent messages and directives regarding public health measures such as wearing face masks
- Economic hardships and poverty
- Scarcity of available commodities (e.g., foods, paper goods, and personal protective equipment)
- Restrictions on personal liberty
- Constant media coverage of the pandemic and the confusion about the information.
Psychiatric Manifestations of COVID-19
There are
currently several preliminary findings on COVID-19's neuropsychiatric
complications, but, based on the effects of past epidemics of multiple
respiratory viruses, an elevated prevalence of behavioural pathologies as an
unwelcome sequela may be assumed. Not only can SARS-COV-2 infiltrate the brain
and inflict direct disruption to neural networks, but the experience of
possibly fatal and untreatable COVID-19 can cause extreme anxiety, leading to
long-term behavioural modifications or exacerbating an underlying psychiatric
disorder. COVID-19 patients may experience various neuropsychiatric symptoms due
to systemic inflammation, cytokine effects in the CNS, SARS-COV-2 infection of
neural cells, neuroinflammation, glial dysfunction, or aberrant epigenetic
modifications stress-related genes.



.png)
1 Comments